Hepatitis A immunization (vaccine)
Immunization is a process to initiate or augment resistance to an infectious disease. The goal of immunization is to prevent, and in some cases eradicate, potentially serious, life-threatening diseases.
Immunizations

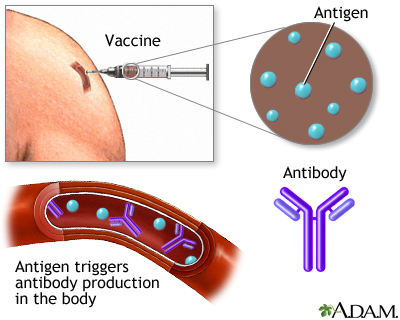
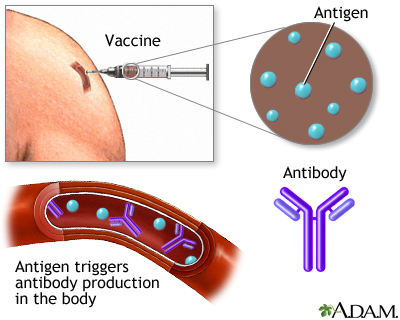
Immunizations (vaccinations) are given to initiate or augment resistance to an infectious disease. Immunizations provide a specialized form of immunity that provides long-lasting protection against specific antigens, which cause disease.
Immunization (vaccination) is a way to trigger your immune system and prevent serious, life-threatening diseases.
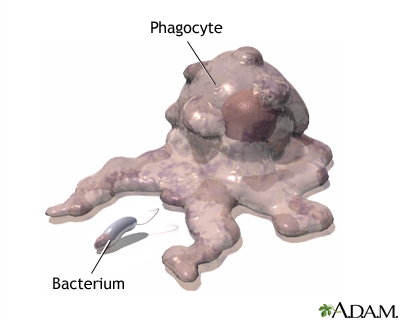
Our bodies are designed to protect us from diseases. When you are exposed to an illness, your immune system actually learns from the experience. The next time your body is exposed to the same illness, your immune system often recognizes the culprit and sets out to destroy it.
Immunization exposes you to a very small, very safe amount of the most important diseases you are likely to encounter at some point in your life. This mild exposure helps your immune system recognize and attack the disease efficiently. If you are exposed to the full-blown disease later in life, you will either not become infected or have a much less serious infection. This is a natural way to deal with infectious diseases.
Throughout human history, infectious diseases have caused measureless misery and death. This rampage was unchecked until the twentieth century, when immunization was introduced on a wide scale. This led to the global eradication of smallpox, the elimination of polio from the Americas, and has almost eliminated tetanus, diphtheria, mumps, and the horrible congenital rubella syndrome. Immunization has greatly reduced the occurrence of measles, pertussis, and meningitis. Millions of deaths and other tragedies have been prevented.
Four different types of vaccines are currently available.
- Attenuated (weakened) live virus is used in the measles, mumps, and rubella (MMR) vaccine and the varicella (chicken pox) vaccine. These vaccines last longer than other vaccines, but may cause serious infections in people with compromised immune systems.
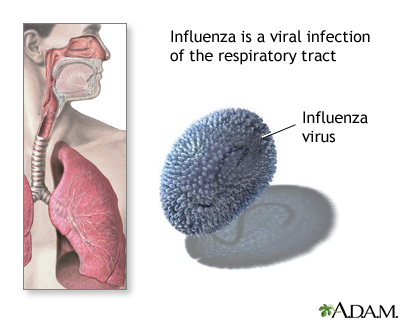
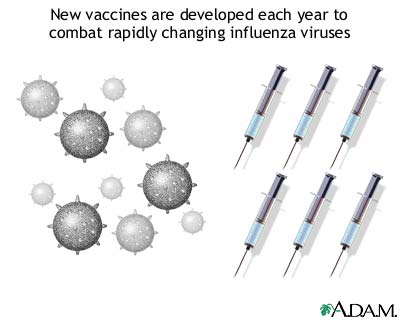
- Killed (inactivated) viruses or bacteria used in some vaccines. For example, the influenza vaccine uses killed virus. These vaccines are safe, even in people with compromised immune systems.
- Toxoid vaccines contain a toxin produced by the bacterium or virus. For example, the diphtheria and tetanus vaccines are actually toxoids.
- Biosynthetic vaccines contain synthetic "man-made" substances which appear to be antigens to the immune system. For example, the Hib (Haemophilus influenzae type B) conjugate vaccine is a biosynthetic vaccine.
IMMUNIZING CHILDREN
Babies get so many shots these days! Many parents are concerned that the sheer number of vaccines might overwhelm, weaken, or use up a baby's immature immune system. But a baby's immune system is built to make antibodies to as many as 10,000 foreign proteins. If a baby were to receive all 11 available vaccines at once, this would engage only a tiny fraction of the immune system.
MERCURY
A small amount of mercury (called thimerosal) is a common preservative in multi-dose vaccines. Despite concerns, thimerosal-containing vaccines have NOT been shown to cause autism or ADHD. Nevertheless, if you have concerns about mercury, all of the routine vaccines are also available without added thimerosal.
IMMUNIZATION SCHEDULE
The recommended immunization schedule is updated at least every 12 months by organizations such as the American Academy of Pediatrics. Consult your primary care provider about specific immunizations for you or your child. At every doctor visit, ask about the next recommended immunizations.
TIPS FOR PARENTS
Immunizations must be given as an injection (shot). The following tips can help make the experience easier for your child:
- Tell older children that the shot is needed to keep them safe and healthy. Knowing what to expect ahead of time may reassure the child.
- Explain to the child that it is OK to cry, but suggest that the child try to be brave. Explain that you do not like injections either, but you try to be brave, too. Praise the child after the injection is over, whether or not he or she cries.
- Distract the child at the moment of the injection. For example, point out a picture on the wall, have them count or say their "ABCs", or tell them something funny.
- Try to be calm. The child will notice if you cringe before the shot!
- Plan something fun to do afterward. A trip to the park, eating out, or other entertainment after the shot can make the next one less scary.
IMMUNIZATIONS FOR ADULTS
Immunizations are not only for children. Each year the CDC posts recommended adult immunizations on their website. Go there to learn about tetanus booster shots, the flu shot, hepatitis A and B vaccines, the pneumococcal vaccine, MMR, and immunizations for chickenpox and meningitis.