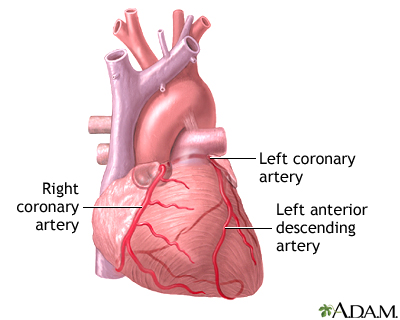
Urine - Bloody
Female urinary tract
The female and male urinary tracts are relatively the same except for the length of the urethra.
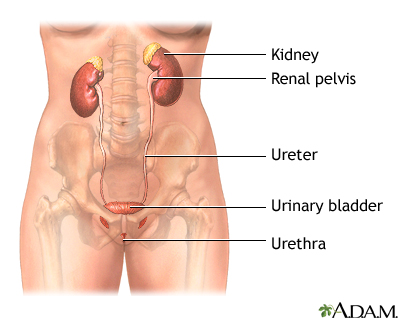
Male urinary tract
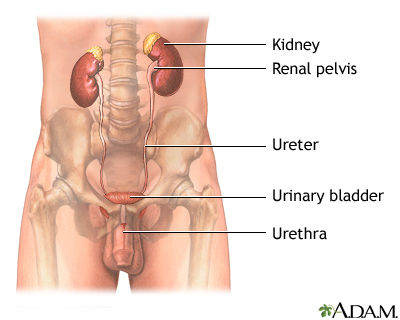
The male and female urinary tracts are relatively the same except for the length of the urethra.
Definition
Blood in your urine, or hematuria, can be classified as microscopic or gross.
- Microscopic hematuria is when there is very little blood in the urine and it can only be seen with a microscope.
- Gross hematuria is when there is enough blood in the urine that you can see it with the naked eye. Uusually it turns toilet water pale pink or bright red, or you may just see spots of blood in the water after urinating.
Considerations
In women, blood may appear to be in the urine when it is actually coming from the vagina. In men, what may be mistaken for urinary bleeding is sometimes a bloody ejaculation, usually due to a prostate problem.
Discoloration from certain drugs, beets, or other foods can mimic blood in the urine.
You may not see blood in your urine. In some cases, it is found microscopically when your doctor checks your urine during a routine exam. Your doctor will follow up on this problem to see if it persists and identify the cause.
When blood is visible to the naked eye, prompt and thorough evaluation is always needed. In children, hospitalization is often necessary to complete the work up.
Common Causes
There are many potential causes of blood in the urine. Often, bloody urine is from a problem in your kidneys or other parts of the urinary tract. If your kidneys, urinary tract, prostate, and genitals turn out to be fine, your doctor may check to see if you have a bleeding disorder.
Kidney and urinary tract causes include:
- Cancer of the bladder or kidney
- Fractured pelvis
- Kidney or bladder stones
- Kidney disease following strep throat ( post-stretococcal glomerulonephritis) -- a classic cause of blood in the urine in children
- Kidney failure
- Infection of the bladder, kidney, or urethra
- Inflammation of the bladder, urethra, or kidney ( glomerulonephritis)
- Injury to the kidney
- Polycystic kidney disease
- Recent urinary tract procedure such as catheterization, circumcision, surgery, or kidney biopsy
Causes from blood disorders include:
- Bleeding disorders (such as hemophilia)
- Blood clot in the kidneys
- Low numbers of platelets
- Medications including blood thinners (such as warfarin)
- Sickle cell disease
Call your health care provider if
Blood in the urine should never be ignored. Tell your doctor about this symptom and get an appropriate evaluation, especially if you have unexplained weight loss, burning with urination, frequent urination, or urgent urination.
Call your doctor right away if:
- You have fever, nausea, vomiting, shaking chills, or pain in your abdomen, side, or back
- You are unable to urinate
- You are passing blood clots
Also call your doctor if:
- You have pain with sexual intercourse or heavy menstrual bleeding -- the problem may be related to your reproductive organs
- You have urine dribbling, nighttime urination, or difficulty starting your urinary flow -- the problem may be related to your prostate
What to expect at your health care provider's office
Your doctor will take a medical history and perform a physical examination. Medical history questions may include:
- When did you first notice blood in your urine?
- What is the underlying color of your urine?
- Do you have any pain with urination?
- Has the quantity of your urine increased or decreased?
- Does your urine have an odor?
- Are you urinating more frequently?
- Do you have an urgent need to urinate?
- What medications are you taking, including over the counter drugs?
- Have you recently eaten foods that may cause discoloration, like beets, berries, or rhubarb?
- Do you have any other symptoms like pain in your back, abdomen, or side? Fever, weight loss, nausea, vomiting, or diarrhea? Nighttime urination? Dribbling? Discharge from penis or vagina? Pain with intercourse?
- Have you had previous urinary problems or kidney problems?
- Do you have any allergies?
- Have you had a recent injury?
- Have you had any recent diagnostic or surgical procedures involving the urinary tract?
Tests that may be done include:
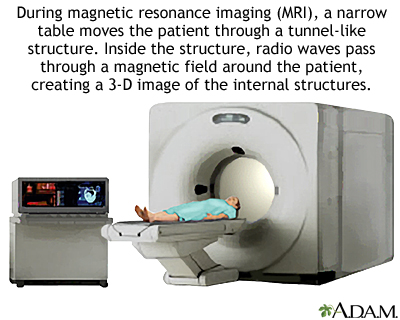
- Abdominal ultrasound
- Blood studies such as a CBC, blood differential, C3, and creatinine
- CT scan of the abdomen
- Cystoscopy
- IVP
- Kidney biopsy
- Kidney x-rays
- Strep test
- Tests for lupus
- Tests for sickle cell, bleeding problems, and other blood disorders
- Urinalysis
- Urine culture
- 24-hour urine collection for creatinine, protein, calcium
The treatment will depend on the cause of the blood in the urine. If a urinary tract infection is confirmed, antibiotics may be prescribed. If appropriate, pain medications will be given.