Breast Cancer
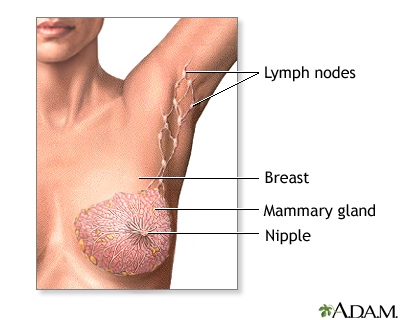
Female Breast

The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Needle biopsy of the breast

A needle biopsy is performed under local anesthesia. Simple aspirations are performed with a small gauge needle to attempt to draw fluid from lumps that are thought to be cysts. Fine needle biopsy uses a larger needle to make multiple passes through a lump, drawing out tissue and fluid. Withdrawn fluid and tissue is further evaluated to determine if there are cancerous cells present.
Open biopsy of the breast

An open biopsy can be performed under local or general anesthesia and will leave a small scar. Prior to surgery, a radiologist often first marks the lump with a wire, making it easier for the surgeon to find.
Breast self-exam
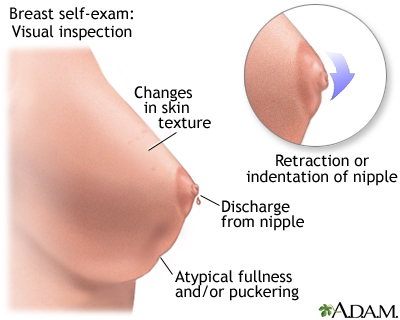
Monthly breast self-exams should always include: visual inspection (with and without a mirror) to note any changes in contour or texture; and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
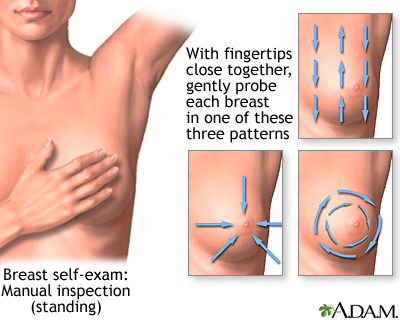
Monthly breast self-exams should always include: visual inspection (with and without a mirror) to note any changes in contour or texture; and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Breast self-exam
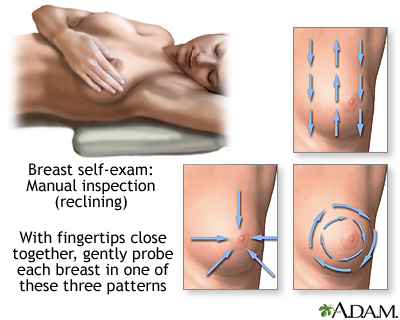
Monthly breast self-exams should always include: visual inspection (with and without a mirror) to note any changes in contour or texture; and manual inspection in standing and reclining positions to note any unusual lumps or thicknesses.
Mammary gland
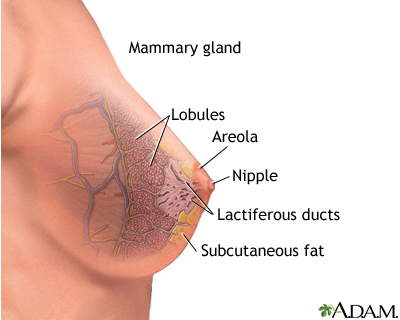
The anatomy of the breast includes the lactiferous, or milk ducts, and the mammary lobules.
Sentinel node biopsy

Sentinel node biopsy is a technique which helps determine if a cancer has spread (metastasized), or is contained locally. When a cancer has been detected, often the next step is to find the lymph node closest to the tumor site and retrieve it for analysis. The concept of the "sentinel" node, or the first node to drain the area of the cancer, allows a more accurate staging of the cancer, and leaves unaffected nodes behind to continue the important job of draining fluids. The procedure involves the injection of a dye (sometimes mildly radioactive) to pinpoint the lymph node which is closest to the cancer site. Sentinel node biopsy is used to stage many kinds of cancer, including lung and skin (melanoma).
Mastectomy - series: Normal anatomy
 |
Breast cancer begins in the breast and spreads first to the lymph nodes of the armpit (axilla). When a breast lump is found to contain cancer, and if the cancer has not spread beyond the nodes of the axilla to distant sites, it is often removed surgically. Radiation therapy may be used in addition to surgery. In certain cases of malignant lumps, lumpectomy followed by radiation therapy is as effective as a radical mastectomy. Typically, lumpectomy does not require a breast replacement (prosthesis).
Breast lump removal - series: Normal anatomy
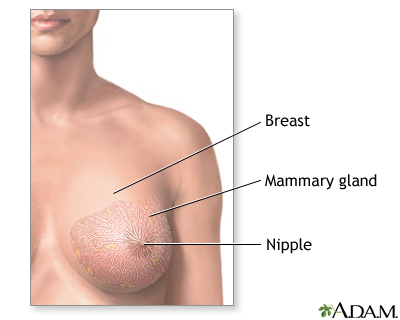 |
The female breast is composed mainly of fatty tissue interspersed with fibrous or connective tissue. The circular region around the nipple is often a different color or pigmented. This region is called the areola.
Definition
Breast cancer is a cancer that starts in the tissues of the breast.
There are two main types of breast cancer:
- Ductal carcinoma starts in the tubes (ducts) that move milk from the breast to the nipple. Most breast cancers are of this type.
- Lobular carcinoma starts in parts of the breast, called lobules, that produce milk.
In rare cases, breast cancer can start in other areas of the breast.
Many breast cancers are sensitive to the hormone estrogen. This means that estrogen causes the breast cancer tumor to grow. Such cancer is called estrogen receptor positive cancer or ER positive cancer.
Some women have what's called HER2-positive breast cancer. HER2 refers to a gene that helps cells grow, divide, and repair themselves. When cells have too many copies of this gene, cells -- including cancer cells -- grow faster. Experts think that women with HER2-positive breast cancer have a more aggressive disease and a higher risk of recurrence than those who do not have this type.
Causes, incidence, and risk factors
Over the course of a lifetime, one in eight women will be diagnosed with breast cancer.
Risk factors you cannot change include:
Age and gender -- Your risk of developing breast cancer increases as you get older. The majority of advanced breast cancer cases are found in women over age 50. Women are 100 times more likely to get breast cancer then men.
Family history of breast cancer -- You may also have a higher risk for breast cancer if you have a close relative has had breast, uterine, ovarian, or colon cancer. About 20-30% of women with breast cancer have a family history of the disease.
Genes -- Some people have genes that make them more prone to developing breast cancer. The most common gene defects are found in the BRCA1 and BRCA2 genes. These genes normally produce proteins that protect you from cancer. But if a parent passes you a defective gene, you have an increased risk for breast cancer. Women with one of these defects have up to an 80% chance of getting breast cancer sometime during their life.
Other genetic defects have been linked to breast cancer, including those found in the ATM gene, the CHEK-2 gene, and the p53 tumor suppressor gene, but these are very rare.
Menstrual cycle -- Women who get their periods early (before age 12) or went through menopause late (after age 55) have an increased risk for breast cancer.
Other risk factors include:
Alcohol use -- Drinking more than 1-2 glasses of alcohol a day may increase your risk for breast cancer.
Childbirth -- Women who have never had children or who had them only after age 30 have an increased risk for breast cancer. Being pregnant more than once or becoming pregnant at an early age reduces your risk of breast cancer.
DES -- Women who took diethylstilbestrol (DES) to prevent miscarriage may have an increased risk of breast cancer after age 40. This drug was given to the women in the 1940s-1960s.
Hormone replacement therapy (HRT) -- You have a higher risk for breast cancer if you have received hormone replacement therapy for several years or more. Many women take HRT to reduce the symptoms of menopause.
Obesity -- Obesity has been linked to breast cancer, although this link is controversial. The theory is that obese women produce more estrogen, which can fuel the development of breast cancer.
Radiation -- If you received radiation therapy as a child or young adult to treat cancer of the chest area, you have a significantly higher risk for developing breast cancer. The younger you started such radiation, the higher your risk -- especially if the radiation was given when a female was developing breasts.
Breast implants, using antiperspirants, and wearing underwire bras do not raise your risk for breast cancer. There is no evidence of a direct link between breast cancer and induced abortion or pesticides.
The National Cancer Institute provides an online tool to help you figure out your risk of breast cancer.
Symptoms
Early breast cancer usually does not cause symptoms. This is why regular breast exams are important. As the cancer grows, symptoms may include:
- Breast lump or lump in the armpit that is hard, has uneven edges, and usually does not hurt
- Change in the size, shape, or feel of the breast or nipple -- for example, you may have redness, dimpling, or puckering that looks like the skin of an orange
- Fluid coming from the nipple -- may be bloody, clear-to-yellow, or green, and look like pus
Men get breast cancer, too. Symptoms include breast lump and breast pain and tenderness.
Symptoms of advanced breast cancer may include:
- Bone pain
- Breast pain or discomfort
- Skin ulcers
- Swelling of one arm (next to breast with cancer)
- Weight loss
Signs and tests
The doctor will ask you about your symptoms and risk factors, and then perform a physical exam, which includes both breasts, armpits, and the neck and chest area. Additional tests may include:
- Mammography to help identify the breast lump
- Breast MRI to help better identify the breast lump
- Breast ultrasound to show whether the lump is solid or fluid-filled
- Breast biopsy, needle aspiration, or breast lump removal to remove all or part of the breast lump for closer examination by a laboratory specialist
If your doctor learns that you do have breast cancer, additional tests will be done to see if the cancer has spread. This is called staging. Staging helps guide future treatment and follow-up and gives you some idea of what to expect in the future.
Breast cancer stages range from 0 to IV. In general, breast cancer that stays where it has started is called in situ or noninvasive breast cancer. If it spreads, it is called invasive breast cancer. The higher the number, the more advanced the cancer.
Treatment
Treatment is based on many factors, including type and stage of the cancer, whether the cancer is sensitive to certain hormones, and whether or not the cancer overproduces (overexpresses) a gene called HER2/neu.
In general, cancer treatments may include:
- Chmotherapy medicines to kill cancer cells
- Radiation therapy to destroy cancerous tissue
- Surgery to remove cancerous tissue - a lumpectomy removes the breast lump; mastectomy removes all or part of the breast and possible nearby structures
Other treatments:
- Hormonal therapy to block certain hormones that fuel cancer growth
- Targeted therapy to interfere with cancer cell grow and function
An example of hormonal therapy is the drug tamoxifen. This drug blocks the effects of estrogen, which can help breast cancer cells survive and grow. Most women with estrogen sensitive breast cancer benefit from this drug. A newer class of medicines called aromatase inhibitors, such as exemestane (Aromasin), have been shown to work just as well or even better than tamoxifen in post-menopausal women with breast cancer.
Targeted therapy, also called biologic therapy, is a newer type of cancer treatment. This therapy uses special anti-cancer drugs that identify certain changes in a cell that can lead to cancer. One such drug is trastuzumab (Herceptin). For women with stage IV HER2-positive breast cancer, Herceptin plus chemotherapy has been shown to be work better than chemotherapy alone. Studies have also shown that in women with early stage HER2-positive breast cancer, this medicine plus chemotherapy cuts the risk of the cancer coming back by 50%.
Cancer treatment may be local or systemic.
- Local treatments involve only the area of disease. Radiation and surgery are forms of local treatment.
- Systemic treatments affect the entire body. Chemotherapy is a type of systemic treatment.
Most women receive a combination of treatments. For women with stage I, II, or III breast cancer, the main goal is to treat the cancer and prevent it from returning. For women with stage IV cancer, the goal is to improve symptoms and help them live longer. In most cases, stage IV breast cancer cannot be cured.
Stage 0 -- Lumpectomy plus radiation or mastectomy is the standard treatment. There is some controversy on how best to treat DCIS.
Stage I and II -- Lumpectomy plus radiation or mastectomy with some sort of lymph node removal is standard treatment. Hormone therapy, chemotherapy, and biologic therapy may also be recommended following surgery.
Stage III -- Treatment involves surgery possibly followed by chemotherapy, hormone therapy, and biologic therapy.
Stage IV -- Treatment may involve surgery, radiation, chemotherapy, hormonal therapy, or a combination of such treatments.
Support Groups
Talking about your disease and treatment with others who share common experiences and problems can be helpful.
Expectations (prognosis)
How well you do after being treated for breast cancer depends on many things. The more advanced your cancer, the poorer the outcome.
The 5-year survival rate refers to the number of patients who live at least 5 years after their cancer is found. According to the American Cancer Society (ACS), the 5-year survival rates for persons with breast cancer that is appropriately treated are as follows:
- 100% for stage 0
- 100% for stage I
- 92% for stage IIA
- 81% for stage IIB
- 67% for stage IIIA
- 54% for stage IIIB
- 20% for stage IV
Complications
New, improved treatments are helping persons with breast cancer live longer than ever before. However, even with treatment, breast cancer can spread to other parts of the body. Sometimes, cancer returns even after the entire tumor is removed and nearby lymph nodes are found to be cancer-free.
You may experience side effects or complications from cancer treatment. For example, radiation therapy may cause temporary swelling of the breast, and aches and pains around the area. Ask your doctor about the side effects you may have during treatment.
Calling your health care provider
Contact your health care provider for an appointment if:
- You have a breast or armpit lump
- You are a woman age 40 or older and have not had a mammogram in the last year
- You are a woman age 35 or older and have a mother or sister with breast cancer, or have already had cancer of the breast, uterus, ovary, or colon.
- You do not know how or need help learning how to perform a breast self-examination
Prevention
Many risk factors -- such as your genes and family history -- cannot be controlled. However, a healthy diet and a few lifestyle changes may reduce your overall chance of cancer in general.
Breast cancer is more easily treated and often curable if it is found early.
Early detection involves:
- Breast self-exams (BSE)
- Clinical breast exams by a medical professional
- Screening mammography
Most experts recommend that women age 20 and older examine their breasts once a month during the week following the menstrual period.
Women between the ages 20 and 39 should have a doctor examine their breasts at least once every 3 years. After age 40, women should a clinical breast exam every year.
Mammography is the most effective way of detecting breast cancer early.
Screening recommendations:
- The American Cancer Society recommends mammogram screening every year for all women age 40 and older. The National Cancer Institute (NCI) recommends mammogram screening every 1-2 years for women age 40 and older.
- If you are high risk, experts say you should start getting a mammogram at age 30. Certain women at high risk of breast cancer should also have a breast MRI along with their yearly mammogram. Ask your doctor if you need an MRI.
- For those at high risk, including those who have or had a close family member with the disease, annual mammograms should begin 10 years earlier than the age at which the relative was diagnosed.
Questions have been raised about the benefit of screening mammography in women under age 50 and over the age of 69. Annual mammograms in women between 50 and 69 have been show to save lives. But while screening can also detect early breast cancer in younger and older women, it has not been shown to save lives.
This is a topic filled with controversy. A woman needs to have an informed and balanced discussion with her doctor, along with doing additional reading and researching on her own, to determine if mammography is right for her.
Women at very high risk for breast cancer may consider preventive (prophylactic) mastectomy, which is the surgical removal of the breasts. Possible candidates for this procedure may include those who have already had one breast removed due to cancer, women with a strong family history of breast cancer, and persons with genes or genetic mutations that raise their risk of breast cancer.
No comments:
Post a Comment